.gif)
Reconstructive Osseous Surgery
Dr. Paulo Camargo:
Definition
"Reconstructive osseous surgery in periodontics is defined as different periodontal surgical procedures directed at restoring bone, periodontal ligament and cementum to their original levels once damaged by periodontal disease."
This does not refer to the restoration of bone only, rather a whole functional attachment apparatus that includes a new periodontal ligament, new cementum and bone.
Modalities of Pocket Elimination


There are four basic modalities of pocket elimination: repair, resection, regeneration and extraction.
The slide on the left shows pocket elimination by repair. Epithelial cells which line the pocket wall will become attached to tooth surface form of a long junctional epithelium once that tooth surface has been made compatible with cell attachment by scaling and root planing.
The slide on the right shows two modalities of pocket elimination:
- From diagram A to B, pocket elimination by resection has been achieved. Pocket elimination by resection can be achieved by surgical removal of the pocket wall (gingivectomy) or by apical displacement of the gingival tissues (apically positioned flaps often combined with resective osseous surgery).
- From diagram A to C, pocket elimination by regeneration or new attachment has been achieved. The regeneration of the whole periodontal unit to its original levels has been achieved. In this lecture pocket elimination by periodontal regeneration will be examined in detail.
A fourth modality of pocket elimination is the extraction of tooth.
Objectives
General objectives of periodontal surgery include: (a) elimination of local factors, (b) elimination or reduction of pockets, (c) restoration of alveolar bone, and (d) regeneration of a functional attachment apparatus.
Over the years, it has been demonstrated that these objectives can be achieved by the insertion of a variety of materials in the bony defect (bone grafts). More recently, it has been demonstrated that these objectives can also be achieved by placing mechanical barriers (membranes) over these defects. The ultimate goal of regenerative periodontal surgery is not only to eliminate pocket depths, but to regenerate a new attachment apparatus and reconstruct the periodontal unit to within previously existing normal physiologic limits. Bone grafts and membranes are steps in this direction.
Indications
As a general rule, periodontal regeneration is limited to areas of VERTICAL bone loss. Some of the most important indications for reconstructive osseous surgery include:
- Deep vertical defects
- Localized Juvenile Periodontitis
- Need for increased bone support
- Anatomical limitations
- Esthetic areas
- Furcation invasions of degree II
Deep vertical defects
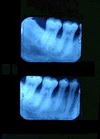
Notice the deep vertical defects on the radiographs. Reconstructive osseous surgery would be best suited in this type of situation. This is primarily due to two major drawbacks potentially associated with an apically positioned flap combined with resective osseous surgery in order to reestablish positive osseous architecture: (a) need for bone removal in the molar furcation area, which would create a furcation invasion that was not present prior to the surgical procedure; (b) extensive removal of supporting bone in the bicuspid area which in this case would mean the resection of approximately 6 mm of supporting bone around the second bicuspid. Therefore, reconstructive osseous surgery was the treatment option for the vertical defects present on the mesial aspects of both molars.
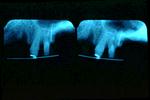
Localized Juvenile Periodontitis

This slide illustrates a typical lesion on a patient with Localized Juvenile Periodontitis (LJP). This lesion is very localized to the first molar and for the same reason as previously discussed, resective surgery was not indicated. Resection would result in extensive loss of supporting bone for both the second molar and the second bicuspid. It is important to mention that patients with LJP usually respond well to Reconstructive Osseous Surgery. This may be due to the following reasons: (a) patient¹s young age and good healing potential and (b) LJP lesions generally present with minimal calculus which facilitates root preparation and increases the potential success of a bone graft or a guided tissue regeneration procedure. On the contrary, patients with adult periodontitis have a significant amount of plaque and calculus on the roots, and proper root instrumentation is more difficult. A limiting factor in vertical defects where reconstructive surgery is indicated, is the ability to perform proper scaling and root planing of the affected area. It is very difficult to access the most apical portion of the defect with a scaling instrument and gain a root surface that is compatible with cell attachment.
Need for Increased Bone Support

The need for increased bone support is another indication for reconstructive surgery. Note the severe loss of bone in this mandibular premolar area. It would be ideal to have the ability to increase the bone support to this tooth which presents with mobility and therefore, be able to retain the tooth for a longer period of time.
Anatomical Limitations
There are anatomical limitations which limit the ability to perform resective osseous surgery.
Proximity to the maxillary sinus may dictate the use of a regenerative procedure versus a resective procedure in order to prevent violation of the sinus area.
Another anatomical limitation is in the area of the external oblique ridge of the mandible. The alveolar ridge can widen towards the buccal and to perform a resective procedure would require reflecting a flap that involves the entire cheek area.
Esthetic Areas

In esthetic areas such as the one illustrated in this slide, the options are to treat the area with a resective or regenerative surgical procedure. If esthetics are not a consideration, a resective procedure would recreate positive architecture and, combined with apically positioning of the soft tissue, pocket elimination would be achieved. However, the result would be a wide interproximal space and teeth would have a "longer" clinical crown. A regenerative approach to this lesion would minimize an adverse esthetic result.
Furcation Invasions

Deep degree II furcation invasions on the buccal of upper and lower molars and linguals of lower molars cannot be treated with a resective procedure since they do not become maintainable. The option available is to try to rebuild the attachment apparatus in the furcation area.
It is important to mention that reconstructive osseous surgery has been shown to have little or no success in interproximal furcation lesions of upper molars or in any degree III furcation invasion.
Limitations
Because of technical reasons reconstructive osseous surgery cannot be performed in areas of horizontal bone loss.
Patient Selection
Prior to performing a regenerative procedure on a patient it is important to consider the following factors:
- Avoid patients with severe medical complications.
- The patient must have a positive attitude towards the treatment. Regenerative procedures are unpredictable and often times require a second surgery. It is important that the patient understands and accepts the limitations of the procedure.
- Regenerative procedures are lengthy. Several follow up visits are necessary and the patient must comply with a rigorous maintenance program especially during the initial phases of healing.
- Finally, and most important of all, the patient must have meticulous plaque control. Although plaque control is important for any type of periodontal therapy, it is critical to the success of a regenerative procedure.
Defect Selection
Factors Related to Success
Another important point in terms of the success of regenerative procedures is the selection of the defect where the procedure will be applied. The following list identifies factors in the selection process that can strengthen procedure outcomes.
Note: Bone grafts require a source of blood supply which is the alveolar bone lining the defect.
- The more bony walls that are in contact with the graft material the better the chances for a successful procedure. The graft material will have an adequate supply of blood and the bony walls will retain the graft material in place.
- Conversely, the more root surface that is in contact with the graft material, the poorer the prognosis of the case because blood supply is limited.
- Narrow defects are better than wide defects. Bone grafts are made up of a material/substance in the form of a paste or powder. Bony walls of a narrow defects work as a "container-like" for the graft material. On the contrary, in a very wide defect the graft material tends to spread or get washed away.


The ideal osseous defect for a regenerative procedure is a 3 wall defect as seen on the distal aspect of this second molar. This defect shape will favor the stabilization of a graft material to be used.
Narrow 2 wall defects are still good indications for reconstructive osseous surgery, but are not as ideal as 3 wall defects.


Interproximal craters, which are common 2 wall interproximal defects, may be an indication for reconstructive osseous surgery if the defect is narrow. Wide craters such as the one seen on the slide respond better to osseous resection than periodontal regeneration.
One wall defects such as the one present on the mesial aspect of this maxillary first molar are poor indications for periodontal regeneration since it is difficult to stabilize the graft material to be used in its proper place.

Circumferential defects are the ones that involve more than one surface of a tooth. They are also referred to as "troughs". Once again, if they are narrow they may be a good indication for periodontal regeneration whereas wide ones are not.